July 8, 2022
If you’re a Medicare provider, you may treat Blue Cross Medicare Advantage Flex (PPO)SM and Blue Cross Group Medicare Advantage Open Access (PPO)SM members, regardless of your contract or network status with Blue Cross and Blue Shield of Illinois (BCBSIL). That means you don’t need to participate in BCBSIL Medicare Advantage networks or in any other BCBSIL networks to see these members. The only requirement is that you accept Medicare assignment and will submit the claims to BCBSIL.
Flex and Open Access Advantage
Individual members may join the Flex plan. The Group Open Access plan is available to retirees of employer groups.
These plans cover the same benefits as Medicare Advantage Parts A and B plus additional benefits per plan. Members’ coverage levels are the same inside and outside their plan service area nationwide for covered benefits.
The Flex plan includes medical coverage and prescription drug coverage. It doesn’t require member cost share.
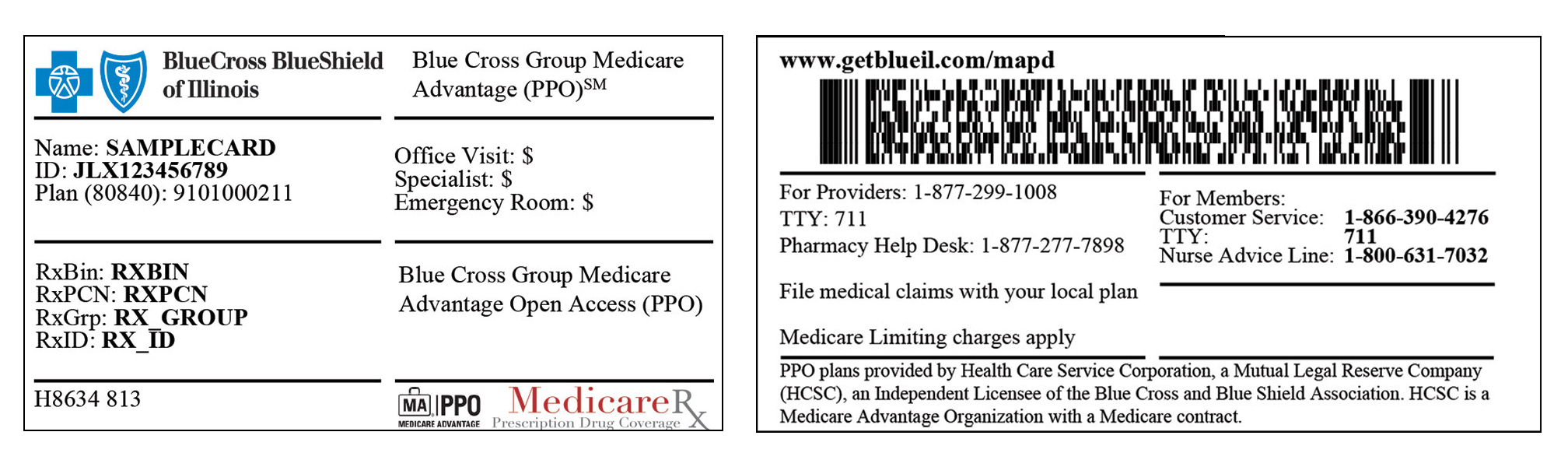
The Open Access plan includes medical coverage and may include prescription drug coverage. Plan members may have to pay deductibles, copays and coinsurance, depending on their benefit plan. Call the number on the member ID card for details.
Referrals aren’t required for office visits. Prior authorization may be required for certain services from Medicare Advantage-contracted providers with BCBSIL. Before providing care to our members, always check eligibility and benefits first.
For reimbursement
Follow the billing instructions on the member’s ID card. When you see these members, you’ll submit the claims to BCBSIL and not Medicare.
If you’re a Medicare Advantage-contracted provider with any Blue Cross and Blue Shield (BCBS) plan, you’ll be paid your contracted rate. You’re required to follow utilization management review requirements and guidelines.
If you’re a Medicare provider who isn’t contracted for Medicare Advantage with any BCBS plan, you’ll be paid the Medicare-allowed amount for covered services. You may not balance bill the member for any difference in your charge and the allowed amount.* You aren’t required to follow utilization management guidelines; however, you may request a review to confirm medical necessity.
Flex plan members
You can identify Flex plan members by their member ID card. Look for the Flex plan name on the front. If you have questions, call 877-774-8592.