Posted March 27, 2023 [Updated May 12, 2023]
This notice has been updated to include additional clarification under the ‘Redetermination Timeline’ and ‘Reinstatement Period’ headers.
Some of your patients could lose their Illinois Medicaid benefits if they don’t complete their redetermination paperwork on time. Unfortunately, your patients may not be familiar with the redetermination process or how it applies to them.
Redetermination Timeline
Congress passed a spending bill in December 2022 that set an end date for the Medicaid Continuous Coverage Requirement. The state of Illinois will again require individuals to redetermine their eligibility for Medicaid coverage. For people who enrolled in Medicaid during the COVID-19 pandemic, this may be their first renewal/redetermination process. Members’ redetermination dates differ. The Illinois Department of Healthcare and Family Services (HFS) will send letters to current Medicaid members to alert them when they need to complete their renewal.
Reinstatement Period
Members that do not submit their redetermination on time have a 90-day reinstatement period. If their redetermination is completed within the 90-day period, and if the member is determined eligible for coverage, the member’s Medicaid coverage will be reinstated back to the first date of lost coverage. If the reinstatement is processed within the 90-day period, the member will be reassigned to the same managed care organization (MCO) prospectively. Providers should bill HFS for any services performed for the period of reinstated coverage.
Plan Termination
Members will be terminated from Medicaid if they don’t complete and return required forms by the end of the 90-day reinstatement period. Members who are non-eligible will be removed from Medicaid and must enroll in an alternate health plan for coverage.
How You Can Help
We need your help to reach people who have Medicaid!
- Please encourage members to follow the steps below to ensure they receive and complete their redetermination in a timely manner.
- If a member needs further help, refer them to Manage My Case at abe.illinois.gov, or tell them to call the Department of Human Services Helpline at 800-843-6154.
Thank you for helping to spread the word about the redetermination process. BCBSIL appreciates your partnership to continue providing access to health care within our community.
Here is information you can share with Medicaid members:
Attention Medicaid Members: Don’t risk losing your health insurance!
Illinois is now starting renewals again to see if you are still eligible for Medicaid. Everybody’s renewal date is different, so it is critical that you take the below steps to renew.
1. Click on “Manage My Case” at abe.illinois.gov.
Create or login to your account at abe.illinois.gov to manage your benefits. Online is the best way to connect.
2. Verify your address.
If you use Medicaid, you need to keep your address current. Click on “Manage My Case” and verify your household information under “Contact Us,” or call 800-843-6154.
3. Find your due date (also called a redetermination date).
Check your “Benefit Details” tab at abe.illinois.gov. Do you want reminders when it’s time to renew? Opt-in for text and email alerts in the “Account Management” tab under “Manage your communications preferences.”
4. Watch your mail.
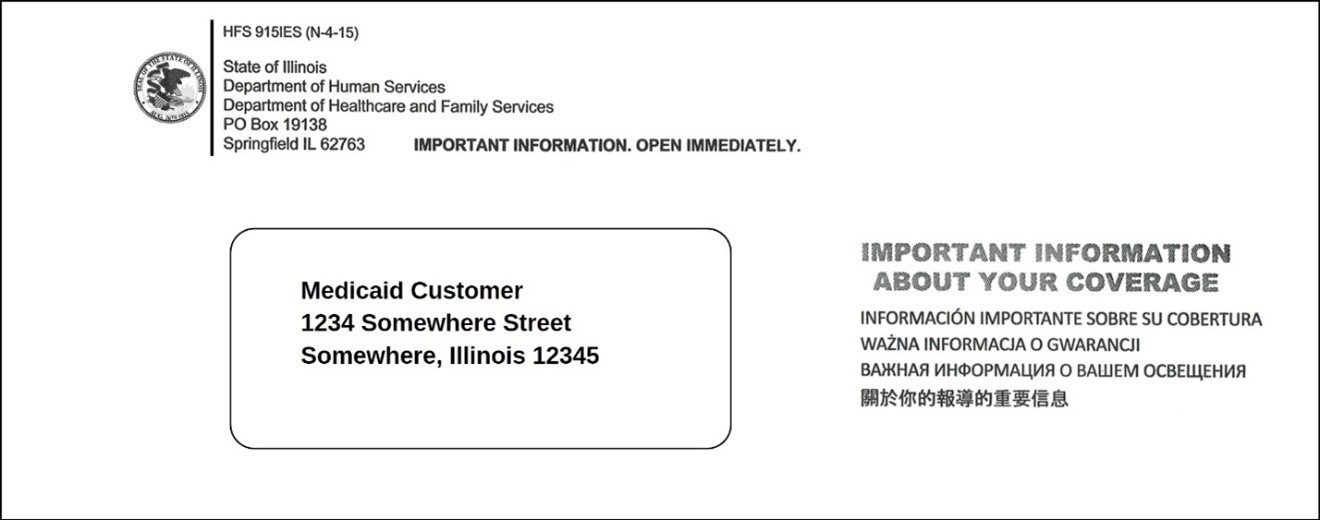
The Department of Healthcare and Family Services (HFS) will mail you a notice to tell you your status and if you need to complete a renewal form. If you have to renew, you will get a renewal a month before it is due. The envelope will look like this:
5. Complete your renewal.
If your letter from HFS says that you need to complete and submit your renewal before the due date (also called redetermination date), to avoid losing your Medicaid benefits, please do so. To renew, go to abe.illinois.gov and select “Manage My Case,” mail your form according to instructions in the letter, or call 800-843-6154.
6. Connect to coverage.
If you are no longer eligible for Medicaid, it is important to quickly get other health insurance to avoid a lapse in coverage.
You can ask your employer if health insurance is offered or you can visit Getcovered.illinois.gov to shop for quality, affordable coverage provided under the Affordable Care Act (ACA). You usually have 30-60 days to enroll in a new plan. This is called a "Special Enrollment Period.”
Get Covered Illinois is the official ACA Health Insurance Marketplace for the state of Illinois, helping you shop for health insurance to fit your needs and budget. Health plans offered on the ACA Health Insurance Marketplace cover pre-existing conditions and essential health benefits, including preventive care and mental health services.
Visit getcoveredillinois.gov for more information, free enrollment assistance, and to find out if you may qualify for financial help. Many people find plans for $10 or less per month after tax credits.
Need more information? Visit abe.illinois.gov or call the Department of Human Services Helpline at 800-843-6154.